Statement of immediate research goals:
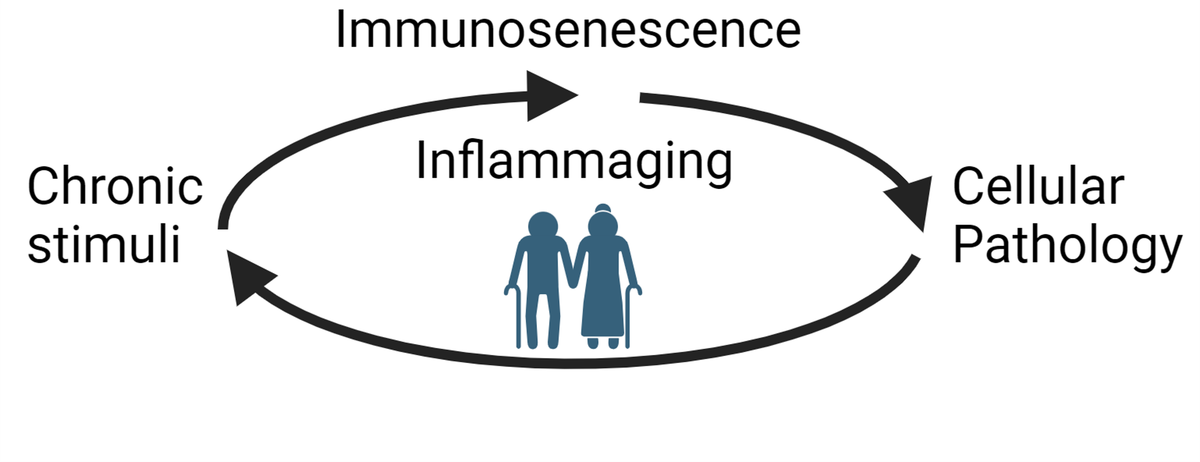
The aging population, defined as individuals that are 65 years of age or older, is expected to double in size over the next 30 years. The COVID 19 pandemic vastly increased public awareness of the susceptibility for older individuals to increased morbidity or mortality during infection with SARs-COV2 and other infections. Despite extraordinary advances in vaccine development and infection transfer, why older people are more susceptible to infections is poorly defined. Hyperactivation of the immune system is an underlying feature. Along with this elevated baseline in inflammation, the immune system of older individuals is unable to appropriately function. My lab investigates the aging immune system to understand how age leads to a decline in organ function and increased susceptibility for infectious diseases.
We have two overlapping focus areas. The first is titled “Manipulating immune-adipocyte interaction to improve energetic substrate availability”. This stems from my discovery that immune cells within a non-lymphoid tissue, the adipose tissue (AT), regulate the lipolytic pathway during aging. We are systematically testing out roles for specific immune cells and identifying the methods by which their deteriorated function can be improved.
We demonstrated that a hyperinflammatory state in old organisms contributes to increased mortality in response to infection relative to young mice (1). We also discovered that there is an accumulation of aged adipose B cells (AABs) and inflammatory macrophages in AT of old mice (2,3). We showed that these immune cells inhibit lipolysis, a metabolic pathway essential for maintaining energy homeostasis. Lipolysis is also necessary to keep inflammation in check in mice challenged with lipopolysaccharide (LPS), a bacterial pathogen-associated molecular pattern from gram-negative bacteria (4). Together these studies support the premise that age-related inflammation mediated by the AT contributes to risk of sepsis. My research seeks to identify how signaling events from AT immune cells, which regulate lipolysis in adipocytes, are altered with age and sepsis. This study could reveal therapeutic targets for improving the response of the elderly. In white adipocytes, lipolysis is activated by two pathways. The canonical pathway responds to local production of catecholamines, which bind the β3-adrenergice receptors (AR), activating PKA and the enzymatic activity of hormone-sensitive lipase (HSL). The non-canonical pathway is activated by LPS binding TLR4, which stimulates ERK and thereby HSL. Activation of the adipocyte lipases (ATGL and HSL) causes triglyceride hydrolysis into free fatty acid. Serum lipid profiles undergo significant changes during infection, and can be used to separate septic survivors from non-survivors 5. Macrophages in AT are a heterogenous population of cells that serve multiple functions, including clearance of FFA, catecholamines and surveillance of the tissue environment. LPS challenge activates a subset of AT macrophages, which release inflammatory cytokines (TNFα and IL-1β). This is significantly amplified in old mice compared to young. Despite the amplified inflammation, the lipolytic pathway cannot be turned on (4). This points towards a new mechanism that could regulate morbidity during sepsis. My research program proposes to dissect the molecular mechanisms driving altered cellular cross-talk. Long term goals will also incorporate projects to investigate organ cross-talk. (Funded by R01AG079913)
In the second research focus, “Therapeutics to modulate immune cell functionality during lethal microbial infection” a project that resulted from collaborations with colleagues, Drs. Laura Niedernhofer, Paul Robbins, Steve Jameson and Sara Hamilton Hart, at the Institute on the Biology of Aging and Metabolism and the Center for Immunology revealed that NME exposure in old mice leads to 100% mortality. This is preceded by a cytokine storm and increased immune infiltrates in multiple tissues. We have demonstrated that the lethality in old NME-exposed mice can be reduced by therapeutics to target cell types that accumulate in old mice. Our recent progress focuses on exhausted T cell subsets during aging and addresses whether checkpoint blockade improves functionality or increases T cell inflammation (5). Ongoing projects will address how the accumulation of senescent cells impacts the quality of the immune response using single-virus, mouse models of aging (funded by P01AI172501; With Steve Jameson, Dave Masopust).
Citations:
1. Camell CD, Sander J, Spadaro O, Lee A, Nguyen K, Wing A, Goldberg E, Youm YH, Brown CW, Elsworth J, Rodeheffer MS, Schultze JL, Dixit VD. Inflammasome-driven catecholamine catabolism in macrophages blunts lipolysis during ageing. Nature. 2017; 550 (7674): 119-23.
2. Camell CD, Lee A, Günther P, Goldberg E, Spadaro O, Youm YH, Bartke A, Hubbard GB, Ikeno Y, Ruddle NH, Schultze JL, Deep VD. Aging induces Nlrp3 inflammasome dependent adipose B cell expansion to impair metabolic homeostasis. Cell Metabolism. 2019. doi.org/10.1016/j.cmet.2019.10.006
3. Camell CD, Yousefzadeh MJ, Zhu Y, Prata LGP…Hamilton SE, Tchkonia T, Niedernhofer LJ, Kirkland JL, Robbins PD. Senolytics reduce coronavirus-related mortality in old mice. Science. 2021. 10.1126/science.abe4832
4. Carey, A., Nguyen,K, Kandikonda, P., Kruglov, V., Bradley, C, Dahlquist, K.J.V., Cholensky, S.H., Swanson, W., Badovinac, V.P., Griffith, T., Camell CD (2024). Age-associated accumulation of B cells promotes macrophage inflammation and inhibits lipolysis in adipose tissue during sepsis. Cell Rep. 2024 Mar 15;43(3):113967. doi: 10.1016/j.celrep.2024.113967. Epub ahead of print. PMID: 38492219.
5. Dahlquist KJV, Huggins MA, Yousefzadeh MJ, Soto-Palma C, Cholensky SH, Pierson M, Smith DM, Hamilton SE, Camell CD. PD1 blockade improves survival and CD8+ cytotoxic capacity, without increasing inflammation, during normal microbial experience in old mice. Nat Aging. 2024 Apr 30. doi: 10.1038/s43587-024-00620-4. Epub ahead of print. PMID: 38689133.